SOGH May 2017 NewsletterThe Society of OB/GYN Hospitalists is dedicated to improving outcomes for hospitalized women and supporting those who share this mission. Comments or Questions about the Newsletter? Contact us!
PRESIDENT'S MESSAGE
It is with great enthusiasm that I announce Vision 2020, SOGH’s first multi-year strategic plan. The Board along with the Society’s Executive Director, Toni Capra, has established goals, priorities and benchmarks for our organization over the next three years. The major focus will be on delineating core competencies which define expectations of practitioners who identify as OB/GYN Hospitalists. In this newsletter’s coding section is a timely article on changes that may impact practitioners via Medicare payment methodology. With such a significant percentage of prenatal care being provided in Federally Qualified Healthcare clinics and with a majority of deliveries being paid for by Medicaid, it is logical to anticipate future change in our practice and compensation. Your feedback is important in helping to proactively shape the role of OB/GYN hospital care. With summer approaching, concern about Zika virus infection in pregnancy is rising. While we can help pregnant women through education about avoiding mosquito bites, reducing risk by avoiding unintended conception remains challenging. One strategy for the most vulnerable population is post placental IUD placement. Until a dedicated postpartum IUD inserter (one has been developed) becomes available, SOGH will continue a skill station at our ACM. While formal training is recommended prior to incorporating this into clinical practice, this protocol (link) for insertion may be informative. For more about copper or hormonal IUD use, as well as other postpartum contraceptive options, please see the CDC Medical Eligibility Criteria Summary Chart. click here.. Hoping to see you at the ACOG Annual Meeting in San Diego. Meredith Meredith Morgan, M.D.President, SOGH
IN THE NEWSPlanning to Attend this year's ACM?As part of SOGH's new strategy to make the event location part of the overall meeting experience, this year's ACM is slated for the international acclaimed city of New Orleans, rich in history, culture and cuisine, and home to the French Quarter, Mardi Gras and jazz. We encourage all attendees to add a day or two at the front or back end of their travel plans to enjoy some of the truly amazing aspects of the Bayou City! The Roosevelt Hotel has promised to honor conference room rates one night prior and one night after the conference! 10 Fun Facts you need to know about the Bayou City!
Learn more about what's in store at ACM 2017!
“CODE THIS!” New Code for Specialist Self Designation by Renée Allen, MD, MHSc., FACOG and Meredith Morgan, MD April 14, 2017
SOGH strives to keep our members abreast of news that impacts our practice as hospitalists; news that you are unlikely to gain through other media. With that in mind, in lieu of a case of the month, “Code This”, has decided to instead share with you new developments within the coding world that may affect our field. As of April 3, 2017, hospitalists can use their own dedicated specialty code. The dedicated code known as C6, allows hospitalists to differentiate themselves from those of outpatient practitioners including internists and family physicians. According to Hospital Medicine, the C6 code may improve the accuracy of tracking hospitalists’ benchmarks such as performance and cost. Current measures fail to consider the unique complexities of the hospitalists’ patients as compared to an outpatient practice. Hospitalists serve patients from all demographics, often with severe illnesses, little available history and limited pre-admission care. Benchmarks used for an outpatient practice simply will not apply for the hospitalist. For this reason, hospitalists may be inappropriately penalized under meaningful use requirements. For instance, when a hospitalist designates a patient encounter as observation, this may be erroneously evaluated as part of an outpatient encounter. This leads to flawed evaluation of quality and cost metrics, which in turn misrepresents the performance and costs associated with being a hospitalist. Having this new code may help shape the Medicare Access CHIP Reauthorization Act (MACRA) and future healthcare policies. Use of the new code by hospitalists is voluntary and its use should not affect billing. The potential information provided by those choosing to employ this new code will provide more accurate metrics for their performance. Benchmarks established by the self-designated specialty population of providers using the code should accordingly reflect the processes and outcomes of the data from those providers. Currently, physicians self-designate their Medicare physician specialty at the time of enrollment in the Medicare program. Per CMS Manual System Pub 100-04 Medicare Claims Processing, Number 9716.04.1, “Contractors shall make all necessary changes to recognize and use the new physician specialty code C6 as a valid primary specialty code or a secondary specialty code for Hospitalist.” While there are a few OB/Gyn hospitalists who limit their practice to OB/Gyn surgery, the number who restrict their practice to internal medicine inpatient care is unknown. SOGH welcomes feedback about any OB/Gyn hospitalists who do limit their practice to inpatient cognitive services (gynecologic or otherwise), internal medicine-type cases, and/or to Medicare beneficiaries such as pregnant patients on dialysis. At the time of this writing, the self-designation status seems to primarily focus on internal medicine (CMS specialty code 11 and hospitalist C6). There are 59 physician specialty codes including 16 which designate obstetrics and gynecology. Currently the Center for Medicare and Medicaid Services (CMS) states “MLN article: A provider education article related to this instruction is available at http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/ .“ The option for OB/Gyn hospitalist to self-designate primary and secondary specialties is available. However, it may be prudent to await analysis of the aforementioned MLN article to determine the use of C6 as primary and 16 as secondary as opposed to 16 as primary and C6 as secondary. Until then, it seems logical that OB/Gyn hospitalists medical claims will be in the 16 specialty designation. Currently, the impact of changing from one’s established designation is unclear. The C6 designation is strictly for usage with CMS (Medicare/Medicaid/tri-care) services databases. When enrolling into the Medicare/Medicaid program, it is up to the provider or practice to self-designate what specialty to which they most closely align themselves. Providers may change their specialty designation through the Medicare enrollment application (Form CMS-8551) or through CMS’ online portal (Provider Enrollment, Chain, and Ownership System, or PECOS). As this does affect how data is tracked, the self-designation may impact flagging of “over/under usage” in additional data and claims that are pulled through the CMS system by providers. Private third-party payers are not obliged to follow those guidelines. Your thoughts on self-designation as a hospitalist are welcome. Please complete and submit this form. Feedback and analysis will be published in a future newsletter. Dr. Meredith Morgan, serves as President of SOGH Dr. Renée Allen is the SOGH Liaison to the ACOG Committee on Health Economics and Coding, Chair of the SOGH Coding Committee and Co-Chair of the SOGH Development Committee. She currently works as an OB/GYN Hospitalist with Mednax/Obstetrix at Eastside Medical Center in Snellville, Georgia.
Sim CornerMagnesium Sulfate Toxicity Presented by Carrie Johnson, MD February 22, 2017
Case Summary: 31 y/o G1 P0 @37 weeks gestation who presented with complaints of severe headache and visual changes. Shortly after arrival in triage, the patient has a witnessed seizure. Per usual hospital protocol, 4gm IV magnesium sulfate loading dose followed by 2gm/hour IV maintenance dose are administered. Within the first hour after admission, the patient has another seizure and receives an additional 2gm IV bolus of magnesium sulfate.
Length: 10-15 minutes Target group: Obstetricians, Midwives, Nurses Possible Team Members for Scenario:
Scenario Specific Goals:
Patient Case Summary:
Mrs. Maggie Magenta is a 31 y/o G1 admitted with the diagnosis of eclampsia. After 24 hours of labor she delivered vaginally without complications.Additional Information:
Set Up
Equipment:
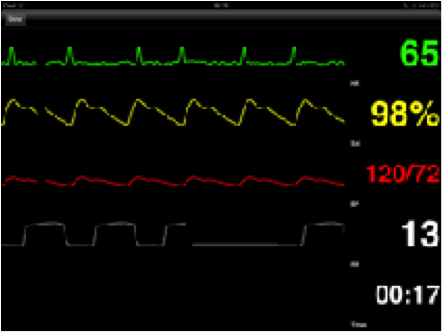
(SimMonitor app, $12.99)
Sequence of Events: 1. Family calls out that patient is having trouble breathing. (Patient and family member are in the room) 2. RN # 1
Debrief:
Magnesium Toxicity Review:Magnesium sulfate is considered a high alert medication, requiring pharmacy premixing and independent verification of the dose and rate prior to initiation. Most institutions have a nursing policy on administration to cover the specifics. But in general:
Signs of magnesium sulfate toxicity: * Absent DTRs * RR < 12 * SOB * Respiratory Arrest * Chest Pain * Coma * Significant drop in BP *Urine Output < 30cc/hour * Signs of Fetal Distress Magnesium Levels
Calcium gluconate is the antidote for magnesium sulfate toxicity. The standard is to administer 1 ampule IV over 10 minutes. A repeat dose may be given if needed. 1 ampule of Calcium Gluconate =
Patient needs to be on continuous ECG during administration.
Carrie Lynn Johnson, MD is an OBGYN Hospitalist who currently practices in Cleveland, OH area.
|