SOGH September 2017 NewsletterMicah Garb, M.D. and Dayna Smith, M.D.Co-editors, SOGH NewsletterThe Society of OB/GYN Hospitalists is dedicated to improving outcomes for hospitalized women and supporting those who share this mission.Comments or Questions about the Newsletter? Contact us!
 PRESIDENT'S MESSAGE
The lead news item for this month is the announcement of agreement by Consultare Partners to continue providing management services for SOGH. This means that Toni Capra as Executive Director will carry through her duties at the Annual Clinical Meeting. She also will support the initiation of our strategic plan which is being led by Tanner Colegrove, our President Elect. With the support of Janet Burkard, membership operations will flow seamlessly into 2018. Now for a somewhat bothersome but true anecdote: Recently a hospitalist was awakened from a deep post-call sleep at home by the unexpected ringing of the front doorbell. On the porch was a patient who had located the doctor’s residential address through an internet search. The patient had come to ask about her hospital experience. The encounter was resolved with the patient being given information on how to obtain her medical records from the hospital. I have several thoughts regarding this incident.
Continuing on the subject of an individual hospitalist’s wellbeing, one must realistically acknowledge variations in sleep patterns and the stress that accompany a hospitalist’s professional life. When accommodations are made incrementally over a period of time, manifestations of prolonged stress might not be readily perceived. To help in recognition, one could use the self-assessment form here. Excessive and/or rapidly increasing stress might indicate need for assistance. Hospital and medical society physicians’ health committees could be among appropriate choices for help. Of relevance is a session, “Managing Stress, Building Resilience: The Imperative of Self-Care for Health Professionals" at our ACM on Tuesday, September 26th, 2017. Two links for self-help are: Medical Student Stress & Burn Out Ending my last President’s Message, I would like to thank all of the individual members of SOGH for allowing me the opportunity to serve. With Gratitude and Best Regards, Meredith Morgan, MD
IN THE NEWSSOGH Featured in US News & World Report "Hospitals Ramping Up Round-the-Clock Staffing for Pregnancy Emergencies" SOGH President Elect, Dr. Tanner Colegrove, was interviewed for this article, Hospitals Ramping Up Round-the-Clock Staffing for Pregnancy Emergencies. The full article is available online, and an excerpt of her contribution to the article is copied below: "As a hospitalist, I see those low-volume, high-acuity [cases] with a lot more frequency, because I am on labor and delivery all the time," says Dr. Tanner Colegrove, medical director of the OB hospitalist program at Northwestern Medicine Lake Forest Hospital in Illinois. "Above and beyond, what makes a hospitalist different, is the mindset of preparing and expecting emergencies," says Colegrove, who is the president-elect of the Society of OB-GYN Hospitalists, with about 550 member physicians. Much more than just a full-time hospital presence, she says, they offer highly honed skills in complex procedures like vaginal birth after cesarean, or VBAC.
“CODE THIS!” (Case of the Month) Multiple Co-Morbidities in Pregnancy in an Established Patient in the Third Trimester by Lori-Lynne A. Webb, CPC and Renee Allen, MD, MHSc., FACOG
Case Excerpt (summary and narrative of actual case): 31 yo G4P1112 at 34 3/7 weeks EGA (by 8 week ultrasound) presented to L&D with complaints of decreased fetal movement and abdominal pain . On this day she hasn't felt the baby move and came in to OB Triage for evaluation. After arriving she reported that she felt the baby move three times in the first twenty minutes of being monitored. The patient complained of 24 hours of intermittent abdominal pain. When she arrived she was contracting every five minutes; which corresponded to her intermittent abdominal pain. She denied vaginal bleeding or loss of fluid. She reported some recent vaginal discharge evaluated by her private OBGYN and found to be normal (negative wet prep, negative gonorrhea and chlamydia testing). She last had sex 8 weeks ago and her last pelvic exam 2 days ago. Her pregnancy was complicated by cholestasis, and she has been performing regular fetal kick counts. The cholestasis of pregnancy was diagnosed several weeks before this triage visit. She had been on oral ursodiol therapy. The pregnancy was also complicated by morbid obesity, with a BMI 54, macrosomia, and polyhydramnios ( AFI 26 and EFW >90th percentile).. Her first delivery in 2010, was by cesarean section at 41 5/7 weeks for arrest of descent. The operative report was available in her chart. A low transverse incision was documented. Her second delivery was a successful VBAC induced at 36 2/7 weeks. Details of the delivery are documented in the EHR . Triage course: The patient was evaluated for preterm labor with serial cervical exams and a fetal fibronectin (FFN), which was negative. Her initial cervical exam was 2cm and a repeat cervical exam two hours later was unchanged. Antenatal corticosteroids were considered. The patient was coincidentally fasting for previously planned gestational diabetes screening and an order was placed for a fasting glucose and metabolic panel. Her fasting glucose was elevated to 112 mg/dl. A 50gram glucose challenge test was ordered and was also elevated to 189 mg/dl. Given the potential diagnostic confounding effect of corticosteroids, a diagnosis of gestational diabetes was made without further glucose testing. Her systolic blood pressure was elevated intermittently during her evaluation. She denied headache or visual changes. She denied right upper quadrant (RUQ) pain. Her abdominal pain was determined to be contractions. A preeclampsia evaluation was done. HerCMP was normal. Her protein:creatinine ratio was indeterminate at 0.2 and a 24 hour urine collection was started. PObHx: 41 wk C/section for arrest of descent, 36wk IOL/VBAC with cholestasisPMHx: Depression, Morbid Obesity, Anxiety, PCOS, PSHx: PLTCS 2010, Cholecystectomy 2011 Medications: ursodiol, fluoxetine, MVI All: NKDA SoHx: nonsmoker, no alcohol, married x 7 years Physical Examination Gen: appears comfortable, lying in bed and in NAD VS: T 98.4, HR 92, RR 18, BP 106/64, 145/80, 153/78, 141/70, 118/62, 121/69, 103/55, 105/54, 123/73, 106/55 Cardiac: RRR Lungs: CTAB, nonlabored breathing Abdomen: gravid, nontender to palpation Vulva: normal external female genitalia, no lesions Vagina: normal appearing vaginal mucosa, thick mucous discharge. Cervix appears closed. Digital cervical exam: 2/50/-2/s/a with fetal vertex palpable at 07:05, repeat exam unchanged FHR tracing: baseline 140, moderate variability, spontaneous accelerations, no decelerations Toco: initially contracting q2-5 minutes
Results Review
The final diagnosis and assessment provided by the OBGYN Hospitalist was:
Follow up with her own private OBGYN is scheduled for 3 days after this triage visit. As the OB hospitalist, how would your services be coded? ANSWER: ICD 10 Diagnosis Coding considerations include: ICD10-CM O24.419 Gestational Diabetes ICD10-CM O13.3 Elevated blood pressure affecting pregnancy in third trimester, antepartum ICD10-CM O47.03 Preterm uterine contractions in third trimester, antepartum ICD10-CM O26.613 Cholestasis of Pregnancy (Liver and biliary tract disorders in pregnancy third trimester ) Z3A.34 34 weeks gestation of pregnancy Evaluation and Management Codes (E&M) 99214-25 CPT codes 59025-26 The Fetal NST CPT code is 59025 with modifier 26 (professional component) – reading and interpretation by physician only. Coding Brief The OB/GYN hospitalist in this case correctly assigned, based on the patient’s presenting history, signs, symptoms and clinical examination, diagnoses of gestational diabetes, preterm uterine contractions, elevated blood pressure affecting pregnancy in third trimester and cholestasis of pregnancy. Under ICD-10, any pregnancy complication diagnosis code must be accompanied by a code in the Z3A family, specifying gestational age. Also per the ICD-10 guidelines, if the trimester is known, it is to be coded, in addition to the weeks of gestation. In this case Z3A.34 denotes 34 weeks gestation. An established patient is defined as an individual who has received professional services from a doctor or another doctor of the exact same specialty and subspecialty who belonged to the same group practice within the past three years. Providers must use procedure codes 99211, 99212, 99213, 99214, and 99215 when billing for established patient services provided in the office or an outpatient (OB Triage) or other ambulatory facility. In the case of OB triage, if this patient was seen by any member of the OBGYN Hospitalist team on a previous date within the last 3 years, these codes would be applicable. Usually the presenting problems that support CPT code 99214 are of moderate to high severity office or other outpatient established patient visit. Counseling and or coordination of care with other providers or agencies are provided as well. . In addition, as with all E&M encounters, a face-to-face encounter is always required. The American Medical Association (AMA) describes the 99214 CPT procedure code as follows: “Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: A detailed history; A detailed examination; Medical decision making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of moderate to high severity. Physicians typically spend 25-45 minutes face-to-face with the patient and/or family.” The 99214 CPT code can be used for time based billingwhen certain requirements are met. However, documentation of time is not required to remain compliant with CMS regulations. If billed without time as a consideration, CPT 99214 documentation should comply with the rules established by the guidelines referenced above. The three important coding components for an established outpatient clinic note are the:
Appropriate documentation for this type of encounter requires TWO out of THREE of the following :
For all established office patient billing codes (99211-99215), the highest documented two out of three above components determines the correct level of service code. Compare this with the requirement for the highest documented three out of three above components for new office patient care encounters (99201-99205). Again, only the highest two out of three components are needed to determine the correct level of care for CPT 99214. Modifier 25 may be used to identify a significant, separately identifiable E&M service performed by the same physician on the same day as another procedure or service. Specifically, the American Medical Association (AMA) Current Procedural Terminology (CPT) book defines Modifier 25 as a Significant, Separately Identifiable Evaluation and Management Service by the Same Physician on the Same Day of the Procedure or Other Service: It may be necessary to indicate that on the day a procedure or service identified by a CPT code was performed, the patient’s condition required a significant, separately identifiable E&M service above and beyond the other service provided or beyond the usual preoperative and postoperative care associated with the procedure that was performed. This modifier is not used to report an E&M service that resulted in a decision to perform surgery. In this case, the NST interpretation also occurred on the same days as the evaluation for abdominal pain and decreased fetal movement. Documentation that supports the provision of a significant, separately identifiable E&M service must be maintained in the client’s medical record. And as always, the OB Hospitalist’s documentation has to support the claim that is billed to the insurance carrier. Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, COBGC and ICD10 CM/PCS Ambassador/Trainer is an E&M, and Procedure based Coding, Compliance, Data Charge entry and HIPAA Privacy specialist, with over 20 years of experience. Lori-Lynne’s coding specialty is OB/GYN office & Hospitalist Services, Maternal Fetal Medicine, OB/GYN Oncology, Urology, and general surgical coding. She can be reached via e-mail at [email protected] or you can also find current coding information on her blog site: http://lori-lynnescodingcoachblog.blogspot.com/. Dr. Renée Allen served as co-author of this column. She is Chair of the SOGH Coding Committee and is the SOGH Liaison to the ACOG Committee on Health Economics and Coding. She currently works as an OB/GYN Hospitalist with Mednax/Obstetrix at Eastside Medical Center in Snellville, Georgia. Questions regarding this case? Contact us at:
Sim Corner Fire in the OR Vanessa Torbenson
September, 2017
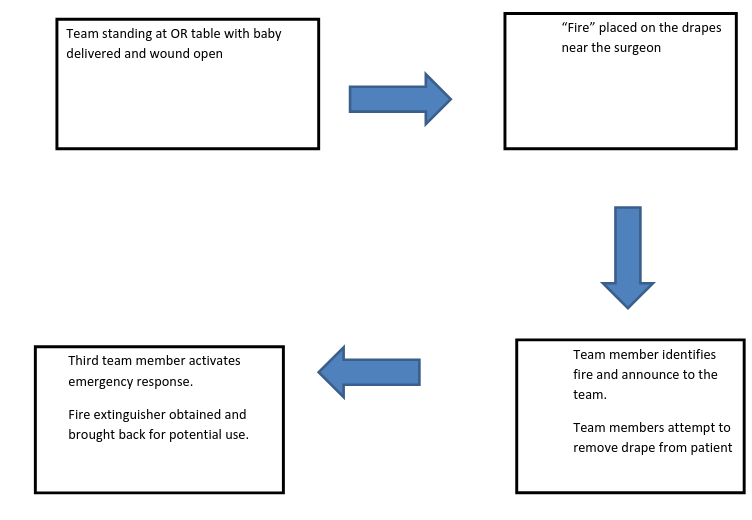
Case summary: Length 10-15 minutes Cesarean delivery Target group: Obstetricians, Anesthesia, Nurses Team members for the Scenario: Obstetrician Anesthesia Scrub RN Circulating RN Patient Family Member General Learning Objectives
Scenario specific Goals:
Debriefing overview:
June is a 37 y/o G2P1001 who is prepped and draped for a repeat cesarean section due to failed TOLAC. The cesarean delivery category is semi-urgent. The team assembles in the OR and performs the routine preoperative safety checks and the time-out. The case is started as per usual. Shortly after the neonate has been delivered and uterus and fascia, but not the subcutaneous tissue is closed, a fire erupts on the drapes adjacent to the surgeon. Additional Information:
Set up: Patient (staff or mannequin) in OR bed with Cesarean delivery drapes placed. Large bright orange flames made out of orange/red felt or construction paper with adhesive tape applied. This is attached to area where flames erupt (Above waist vs below waist) Equipment:
Sequence of Events:
Teaching Points: 1) Drapes to be removed right away if possible 2) Discuss the RACE mnemonic ( Rescue –Alarm- Contain-Extinguish) 4) Discuss the PASS mnemonic ( Pull-Aim-Squeeze-Sweep) 5) Knowledge of activation of fire emergency 6) Knowledge of local fire alarms and extinguishers 7) Examine patient for burns 8) Maintain communication with patient and family Debrief:
Calibrate --> Identify and correct misconceptions Reference: "Resources and Tools for Preventing Surgical Fires, US, FDA"
ACM 2017: General Session Faculty Offer
Expertise, Insight, and Innovation.
by 2017 ACM Co-Chairs The 2017 Annual Clinical Meeting is right around the corner and we are looking forward to meeting you all in New Orleans. Thank you to those who have already registered, and for those that haven't---there's still time.
We are excited to announce that the American College of Obstetrics & Gynecology will offer Part IV Maintenance of Certification accreditation for the following SOGH Annual Clinical Meeting Workshops:
You will find our SOGH ACM course information on the ABOG site as well. As soon as you complete the course, your information will be submitted to ABOG for credit.
In this newsletter, we would like to introduce our expert speakers who will be presenting on a wide range of topics including emergency triage conditions, teamwork and collaboration, self-care and the future of subspecialty.
Dr. Jennifer Butler, Associate Professor at University of California, Irvine, and Director of the OB/GYN fellowship will discuss the educational future of our subspecialty, explore the curriculum of fellowships and the development of core competencies. [Full Bio] ACM 2017 Course: The Educational Future of Our Subspecialty: Fellowships and Core Competencies
 Dr. Caughey, chair of the Department of Obstetrics and Gynecology and associate dean for Women’s Health Research and Policy at OHSU will address teams in the setting of labor and delivery. [Full Bio] ACM 2017 Course(s): Obstetrician and Midwives: No "I" in Team
 Sue Gardner
Sue Gardner, lawyer and claims specialist, will pair with Dr. Jane van Dis, OB hospitalist and Medical Director of Business Development for OBHG. They will present real case examples to highlight the problems and pitfalls leading to litigation. [Full Bio]
ACM 2017 Course: Learnings from Litigation
 Dr. Elizabeth E. Gerard
Dr. Gerard, Associate Professor of Neurology at Northwestern Memorial Hospital, will highlight one of our triage topics as she discusses the evaluation and management of headaches and seizures in pregnancy. (Full Bio)
ACM 2017 Course(s): Headaches and Seizures in Pregnancy
 Dr. Afshan B. Hameed
Dr. Hameed is a Professor of MFM & Cardiology at University of California at Riverside who also directs Obstetrical Services & Quality and Safety. Her presentation will focus on how to triage a patient presenting with Chest Pain and SOB. [Full Bio]
ACM 2017 Course: Chest Pain and Shortness of Breath in Pregnancy
 Dr. Aviad Haramati
Dr. Haramati, Professor and Director, Center for Innovation and Leadership in Education at Georgetown University will share stress management strategies for building resilience. [Full Bio]
ACM 2017 Course - Plenary Lecture: Managing Stress, Building Resilience: The Imperative of Self-Care for Health Professionals
 David Lagrew, MD
Dr. Lagrew is a MFM specialist and physician informaticist with a special interest in maternal quality improvement. He will focus on how to improve vaginal delivery rates based on evidence-based medicine. [Full Bio]
ACM2017 Course: The OBGYN Hospitalist Role in Promoting Vaginal Delivery
 Dr. Mark B. Landon
Dr. Landon, Professor and Chairman of the Department of OB/GYN at Ohio State University College of Medicine and internationally recognized authority on diabetes in pregnancy will discuss recognition and treatment of DKA. [Full Bio]
ACM 2017 Course: Diabetic Ketoacidosis
 Dr. Elliot Main
Dr. Elliott Main is a MFM specialist, Medical Director and Executive Committee Chair of the California Maternal Quality Care Collaborative and will be discussing implementation of National Safety Bundles. [Full Bio]
ACM 2017 Course: Implementation of National Safety Bundles: Your role as a Hospital Quality Leader
 Christian M. Pettker, MD
Dr. Pettker, MFM and Chief of Obstetrics at Yale-New Haven Hospital and Yale School of Medicine will review the fundamental of care for pregnant patients in the ICU. [Full Bio]
ACM 2017 Course: Keeping it Safe When Things Get Critical: Fundamentals of Care for Pregnant Patients in the ICU
 Dr.Scott A. Shainker, DO, MS
Dr. Shainker is the co-founder and director of the New England Center for Placental Disorders, a regional referral center for patients with invasive placentation. He will share his expertise in management of the unexpected invasive placenta. [Full Bio]
ACM 2017 Course: Management of the Unexpected Placenta Accreta
Patrice M. Weiss, MD, is Executive VP and CMO at Carilion Clinic as well as Professor of OB/GYN at the Virginia Tech SOM. As an expert on The Second Victim, she will be sharing strategies for coping with medical error and its toll on OB/GYN physicians. [Full Bio] ACM 2017 Course: The Second Victim
ACM 2017 Workshops Feature All-Star Faculty LineupWe are excited about our line-up of dynamic and talented speakers planned to lead this year's ACM Workshops. We chose instructors who are at the top of their fields and known for bringing innovative and creative strategies to the real-life situations we face daily as OB/GYN's and physicians. Dr. Pare joins us from Oregon Health & Science University, where she is a Maternal Fetal Medicine specialist. Dr. Pare also coordinates the resident Ob Simulation and Skills program. She has a passion for operative vaginal delivery, especially forceps and works with others to assure safe use. Dr. Pare’s course will offer a one-hour lecture reviewing the principles of safe operative vaginal delivery for both forceps and vacuum. The lecture will be followed by a skills session allowing hands on for all participants using an instrumental delivery pelvic trainer to provide a realistic experience. [ACM Faculty Page]
 Dr. Jeffrey Dungan
Dr. Dungan is an Associate Professor of Clinical Genetics and Director of Ob/Gyn Ultrasound at Northwestern University. Dr. Dungan will offer a hands-on course covering common clinical scenarios encountered by the ObGyn hospitalist across the gestational-age spectrum. Ultrasound simulation stations will be used for hands-on practice and assessment. [ACM Faculty Page]
 Dr. Aviad Haramati
Dr. Aviad Haramati is Professor of Integrative Physiology of the Department of Biochemistry, Molecular and Cellular Biology and Department of Medicine at Georgetown. He is the Director of Center for Innovation and Leadership in Education (CENTILE). Dr. Haramati will offer both a plenary session and as a workshop addressing stress management and resilience building for health professionals. The goal of Dr. Haramati’s workshop is to introduce participants to the reality of stress and burnout, to gain insight from the physiology of stress, and to give participants an opportunity to experience several mind-body medicine skills to gain insight to their impact and utility. [ACM Faculty Page]
 Dr. Sean Esplin
Dr. Sean Esplin is an Associate Professor of Obstetrics and Gynecology at the University of Utah. Dr. Esplin's main areas of interest are the genetic control of term and preterm labor and the role of inflammation in preterm birth and he is currently involved in several ongoing research projects sponsored by the NIH aimed at identifying markers of preterm birth and obstetric complications. He also has an interest in Fetal Heart Rate Interpretation and is currently involved in several funded studies designed to evaluate protocols for interpretation and intervention on continuous FHR monitoring. [ACM Faculty Page]
Andrea K. Schneider is a Professor of Law at Marquette University Law School where she specializes in Negotiation, Ethics, and International Conflict Resolution. She is author and co-author of numerous books in the field of dispute resolution and currently serves as co-chair of the editorial board of the ABA Dispute Resolution Magazine and on the Board of Advisors for the Saltman Center for Conflict Resolution at UNLV School of Law. Her most recent accolade, a 2017 award from ABA Section of Dispute Resolution Award for Outstanding Scholarly Work. She speaks nationally and internationally, to non-profits, corporations, law firms, and court systems and others. Most recently she has focused on faculty in the STEM and medical fields for which she has received federal grants for software development and training. Her session with SOGH will examine conflict styles, how to identify style and strategy in others, and how to negotiate effectively on behalf of one’s self or organization. [ACM Faculty Page] ACM 2016 Poster Contest WinnerCongratulations to last year's ACM Poster Contest winner, Adam Crosland!
Adam Crosland, M.D. M.P.H. Resident PhysicianDepartment of Obstetrics & Gynecology University of California, Irvine SOGH will present the 2nd Annual Poster Contest at the upcoming Annual Clinical Meeting in New Orleans. Details of contest participants and the winning poster submission will be announced in the next newsletter. |