SOGH July 2017 Newsletter
Dayna Smith, M.D.Co-editor, SOGH Newsletter
The Society of OB/GYN Hospitalists is dedicated to improving outcomes for hospitalized women and supporting those who share this mission.Comments or Questions about the Newsletter? Contact us!
PRESIDENT'S MESSAGE

SOGH’S Special Interest Group Session at the ACOG Annual Clinical Meeting featured presentations by three of our own members. Brigid McCue discussed informative and practical considerations involved in the initiation and running of an OBED. Tanner Colegrove outlined plans for determining characteristics that would differentiate OB/GYN hospitalists’ practices from other providers of women’s services in the hospital setting. Cate Stika provided the final results from the SOGH 2016 Employment and Salary Survey. I would personally like to express my gratitude to each of them for their hard work and high quality performance.
Information in our survey includes demographics of our practitioners, statistics related to volume of workload, benefits, and compensation data. If you didn’t receive the survey via your email, the report is available free to SOGH members by logging into the SOGH website and accessing it through the Resources section. The extra effort put forth to participate by all respondents and everyone involved in such a large project is greatly appreciated.
The important reasons for SOGH having been formed as an independent organization were the ability to address issues highly specific to our practice and the capability to do so when time is an important factor. An idea that might be associated with a highly functioning OB/GYN hospitalist could be the use of mental checklists in unusual circumstances where intensity might result in those otherwise preoccupied omitting a potentially beneficial option, particularly if that action might only develop utility in the future. For example: After delivery with an Apgar <3 result, the neonatologist/pediatrician would be appropriately focused on resuscitation and infant care including possible transfer and use of a cooling protocol to reduce risk of hypoxic-ischemic encephalopathy. The OB/GYN hospitalist’s remembering to include cord blood specimen collection for possible future stem cell therapy might potentially give hope when support is needed. If this concept interests you, it should prove informative to read Gonzales-Portillo’s article in Frontiers of Neurology “Stem Cell Therapy for Neonatal Hypoxic-Ischemic Encephalopathy”
Best Regards,
Meredith Morgan, M.D.
President, SOGH
e-mail
IN THE NEWS
SOGH Members Featured at ACOG National Summit on Women's Health
by Jennifer Butler, M.D., Associate Professor at the University of California, Irvine
 Along with my colleagues, Cate Stika and Tanner Colegrove, I had the privilege of representing SOGH at ACOG’s National Summit on Women’s Health. Discussion focused on the future of our specialty, patient advocacy and resident education. Concerns were raised about the increased amount of information residents need to learn compounded by decreased work hours, and the overall effect this has on patient care. Over the past couple of decades, the number of procedures performed by graduating residents has dramatically decreased. For example, the mean number of hysterectomies performed by residents in 1980 was 175-180; in 2015 it was 90. A similar trend can be seen with forceps. The median number of FAVD performed by graduating residents in 2003 was 19 and in 2015 it decreased to five. What does this mean overall? Well, to quote Drs. Berkowitz and Minkoff: “We risk training generalists who know more and more about less and less.” Along with my colleagues, Cate Stika and Tanner Colegrove, I had the privilege of representing SOGH at ACOG’s National Summit on Women’s Health. Discussion focused on the future of our specialty, patient advocacy and resident education. Concerns were raised about the increased amount of information residents need to learn compounded by decreased work hours, and the overall effect this has on patient care. Over the past couple of decades, the number of procedures performed by graduating residents has dramatically decreased. For example, the mean number of hysterectomies performed by residents in 1980 was 175-180; in 2015 it was 90. A similar trend can be seen with forceps. The median number of FAVD performed by graduating residents in 2003 was 19 and in 2015 it decreased to five. What does this mean overall? Well, to quote Drs. Berkowitz and Minkoff: “We risk training generalists who know more and more about less and less.”
A diverse group of OB/GYN leaders from across the country attended this summit and brainstormed about how to improve resident education to produce competent and confident graduates. Some concrete ideas included tracking during the 4th year of residency, increased simulation and improved competency evaluations. This is the beginning of a long journey, but the level of enthusiasm in this group was infectious. The future of our specialty depends on us evolving with the changing needs of our trainees and patients.
SOGH representatives Dr. Tanner Colegrove and Dr. Jennifer Butler attending the ACOG Summit. (Dr. Cate Stika not pictured)
SOGH Partners with Perinatal Quality Foundation

SOGH is pleased to once again partner with the Perinatal Quality Foundation to provide a CLEAR (Cervical Length Education and Review) certification discount for registrants of Dr. Jeffrey Dungan's Ultrasound for the OB/GYN Hospitalist workshop at the upcoming 2017 Annual Clinical Meeting. The CLEAR program is an integrated lecture, exam, and image review program designed to improve sonography cervical length measurements.
The Perinatal Quality Foundation's mission is to support programs and research that will improve the quality of obstetrical care. SOGH is thrilled to collaborate on this invaluable educational opportunity. Details on the workshop and CLEAR discount are available on the ACM webpage. Early registration is encouraged as space in the workshop is limited.
Audio Digest Publishes SOGH 2016 ACM Lecture
Rated five stars, Dr. Brian M. Mercer's class on Preterm Labor, presented at the SOGH 2016 Annual Clinical Meeting is now available for purchase from Audio Digest. You'll find it under Volume 64, Issue 12, June 21, 2017.
“CODE THIS!”
Vomiting in Pregnancy in the Third Trimester
by Lori-Lynne A. Webb, CPC and Renée Allen, MD, MHSc., FACOG
July, 2017
Case Excerpt (summary and narrative of actual case):
29 year old G1 at 34 4/7 weeks EGA by LMP consistent with an 8 week ultrasound, who presented to OB triage with a complaint of chronic vomiting during pregnancy. The patient reported that she had been vomiting intermittently over the last month. She had an episode two days prior to, and again the morning of her triage visit. Her vomiting episodes typically occur in the mornings. The patient reported that the day of admission she ate a breakfast of fruit and granola, then drank water. She then immediately vomited. The patient also reported nausea and mild dizziness. She denied abdominal pain, diarrhea, painful urination, and other symptoms. She denied eating unusual or spicy foods. She reported occasional constipation for which she takes Miralax. She works as a Nurse Practitioner on the Internal Medicine Hospitalist Service and reported many ill contacts.
She reported normal fetal movements and denied vaginal bleeding, leaking of fluid and contractions. She had been seen by her prenatal care provider Dr. P in the office one day prior and advised that if the vomiting continues she should be evaluated in OB triage. As the vomiting recurred, she decided that it was time to come to the hospital for further evaluation.
PMH: Migraines
PSH: 2009- Intussusception, Ileocecal, at age 22 treated with a partial small bowel resection and concurrent appendectomy. Tonsillectomy
Meds: PNV, Miralax
All: NKDA
GYN: no STDs, PID, no h/o abnormal Pap or GYN disorders
OB: G1, Rh negative, current gestation – no other complications
Soc: married x 6 years, husband is an intern in residency. Nonsmoker, no alcohol or drug use
Physical ExaminationGen: appears well and in NAD
VS: BP 127/73, HR 85, afebrile 97.7
Cardiac: RRR
Lungs: CTAB
Abdomen: gravid, non-tender, soft, non-distended, no rebound or guarding, non-acute abdomen
FHR tracing: baseline 135, moderate variability, spontaneous accelerations, no decelerations. Category I Fetal Tracing
Toco: 4 contractions in 70 minutes of observation
Extremities: No edema
Labs
|
|
Sodium Level
|
137 mEq/L
|
|
|
Potassium Level
|
4.1 mEq/L
|
|
|
Chloride Level
|
108 mEq/L
|
|
|
Carbon Dioxide Level
|
21 mEq/L LOW
|
|
|
Glucose Level
|
92 mg/dL
|
|
|
BUN
|
4 mg/dL LOW
|
|
|
Creatinine
|
0.52 mg/dL LOW
|
|
|
ALT/SGPT
|
17 Units/L
|
|
|
AST/SGOT
|
24 Units/L
|
|
|
WBC Count
|
11.09 thou/cumm
|
|
|
Hemoglobin
|
11.6 gm/dL
|
|
|
Hematocrit
|
33.3 % LOW
|
|
|
Platelet Count
|
252 thou/cumm
|
|
|
|
|
A CBC and CMP were obtained. While in OB triage, the patient declined IV fluids and IV anti-emetics. The patient was able to take nap while waiting for her labs to return and reported that she did feel better after resting. She was also able to drink a glass of water and pass an oral challenge test. She had no vomiting episodes during her evaluation. The patient stated that she felt better after observation and indicated that after 1.5 hours of monitoring and observation in OB Triage, she felt that she could return to work.
The final diagnosis and assessment provided by the OBGYN Hospitalist was
1) 29 yo G1P0 female at 34 3/7 weeks with intermittent vomiting in pregnancy x 1 month with one episode recent episode today. Otherwise normal evaluation with no evidence of Preeclampsia
2) Constipation
The patient was discharged home in stable condition with preterm labor precautions, fetal kick counts instructions, instructions to continue taking Miralax as needed for constipation, maintain a BRAT diet for 1 week and instructions to follow up with her local OB/GYN in 5-7 days.
As the OB hospitalist, how would your services be coded?
ANSWER:
ICD 10 Diagnosis Coding considerations include:
ICD10-CM O21.2 Late vomiting of pregnancy after 22 weeks, antepartum
ICD10-CM K59.00 Constipation unspecified K59.00
ICD10-CM Z3A.34 34 weeks gestation of pregnancy
Evaluation and Management Codes (E&M)
99204.25 Office or Other Outpatient Visit for New Patient
CPT codes
59025-26 The Fetal NST CPT code is 59025 with modifier 26 (professional component) – reading and interpretation by physician only.
Coding Brief
The OB/GYN hospitalist in this case correctly assigned, based on the patient’s presenting history, signs, symptoms and clinical examination, a diagnosis of Late Vomiting in Pregnancy and Constipation.
Under ICD-10, any pregnancy complication diagnosis code must be accompanied by a code in the Z3A family, specifying gestational age. Also per the ICD-10 guidelines, if the trimester is known, it is to be coded, in addition to the weeks of gestation. In this case Z3A.34 denotes 34 weeks gestation.
A new patient is one who has not received any professional services from a physician or from another physician of the same specialty who belongs to the same group practice, within the past three years. Providers must use procedure codes 99201, 99202, 99203, 99204, and 99205 when billing for new patient services provided in the office or an outpatient (OB Triage) or other ambulatory facility. New patient visits are limited to one every three years, per client, per provider. Usually the presenting problems that support CPT code 99204 are of moderate to high severity. Counseling and or coordination of care with other providers or agencies are provided as well.
Appropriate documentation for this type of encounter requires THREE out of THREE of the following : 1) Comprehensive History 2) Comprehensive Exam
3) Moderate Complexity Medical Decision-Making
Or, if coding is based on time, physicians typically spend 45 minutes face to face with the patient if employing this particular code.
In contrast, an established patient is one who has received professional services from a physician or from another physician of the same specialty within the same group practice, within the last three years. Providers must use procedure codes 99211, 99212, 99213, 99214, and 99215 when billing for established patient services provided in the office or an outpatient or other ambulatory facility. In the case of OB triage, if this patient was seen by any member of the OBGYN Hospitalist team on a previous date within the last 3 years, these codes would be applicable. The same documentation criteria apply for this type of encounter as noted above for new patients encounters.
Modifier 25 may be used to identify a significant, separately identifiable E/M service performed by the same physician on the same day as another procedure or service. In this case, the NST interpretation also occurred on the same days as the evaluation for vomiting. Documentation that supports the provision of a significant, separately identifiable E/M service must be maintained in the client’s medical record.
Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, COBGC and ICD10 CM/PCS Ambassador/Trainer is an E&M, and Procedure based Coding, Compliance, Data Charge entry and HIPAA Privacy specialist, with over 20 years of experience. Lori-Lynne’s coding specialty is OB/GYN office & Hospitalist Services, Maternal Fetal Medicine, OB/GYN Oncology, Urology, and general surgical coding. She can be reached via e-mail or you can also find current coding information on her blog site.
Dr. Renée Allen served as co-author of this column. She is Chair of the SOGH Coding Committee and is the SOGH Liaison to the ACOG Committee on Health Economics and Coding. She currently works as an OB/GYN Hospitalist with Mednax/Obstetrix at Eastside Medical Center in Snellville, Georgia.
Questions regarding this case? Contact us!

Fellowship Programs Cultivate Leaders
Did you know that there are two OB/GYN Hospitalist Fellowships in the country (and more to come)? First established at Winthrop University Hospital in 2013 and later at the University of California in 2015, these fellowships cultivate leaders in advanced obstetric clinical skills, patient safety, and quality care. Both programs are now accepting applications for the 2018-19 academic year. If interested, contact Dr. Anthony Vintzileos by email at Winthrop University, or Maryann Emery at UC Irvine by e-mail, phone, 714.457.7733, or online.
CLINICAL PEARL
"When You Hear Hoof Beats, Think Horses, Not Zebras".
by Cate Stika, M.D., FACOG
Every student of medicine knows the adage: “When you hear hoof beats, think of horses, not zebras.” While that certainly applies to most patients, every so often it’s important to remember, sometimes, it is a zebra.
A 38yo G4P2012 at 23.4 weeks of gestation presented to Ob Triage with vaginal bleeding. She reported bright red blood on the toilet tissue following both urination and defecation since intercourse 3 nights earlier. Pregnancy history was remarkable for a brief episode of vaginal spotting at 18 weeks but otherwise no other postcoital or spontaneous bleeding. She denied any change in her vaginal discharge, pelvic pressure, or contractions. A second trimester ultrasound showed a fundal placenta. A urinalysis showed 0-3 red blood cells and was otherwise negative. As I prepped for the speculum exam, the classic differential for post-coital vaginal bleeding in the mid-second trimester ran through my mind ( cervical polyp, friable cervical mucosa from a yeast or Trichomonas infection, cervical incompetence, subchorionic bleed, etc).
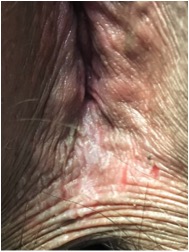
On initial inspection, vulva appeared normal, but on closer inspection after separating the labia majora, the perinal body had diffuse lichenification with hyperkeratosis and multiple vertical fissures that had split during intercourse (see adjacent photo). The remainder of the exam was unremarkable, incl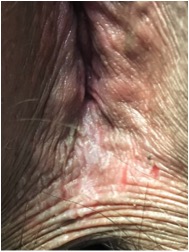 uding wet mount microscopy. uding wet mount microscopy.
I queried the patient regarding symptoms of vulvar itching or irritation at which point she relayed that two weeks prior she had restarted using Summer’s Eve® spray, applying it to her underwear and occasionally directly onto her vulvar skin. She further reported that each time she uses this product, she develops vulvar itching after several weeks and has to temporarily stop using it.
The patient was deemed stable for discharge with the diagnosis of contact dermatitis with resultant bleeding from skin breakdown. She was advised to discontinue all feminine hygiene products and recommended to use an over-the-counter topical hydrocortisone ointment once or twice daily until the fissures healed and the itching resolved. Additionally, she was recommended to apply a small amount of petroleum jelly to the area as needed several times daily to both soothe the skin and to help reduce painful exposure to urine, and rinse with cool water as needed for symptomatic relief.
Discussion:
Contact dermatitis was an unexpected finding in a patient who presents with 2nd trimester bleeding but fortunately a benign and easily treatable condition. For more severe reactions, a mid-to-high potency topical steroid ointment is recommended. Ointments are advised for moist vulvar skin because creams are water soluble and easily wipe off and often contain alcohols which can burn inflamed skin. It is also important to counsel women not to “overwash” because chemicals in soaps, abrasion from vigorous scrubbing and even contact with hot water can be irritating to the delicate vulvar mucosa.
The vulvar skin is particularly sensitive to contact allergens and irritants. The presence of moisture, heat, pockets of occlusion, areas of friction, exposure to urine, as well as the absence of a protective keratin surface within the introitus, all contribute to the increased vulnerability of the vulvar mucosa to topical chemicals. In addition, vulvar contact dermatitis is often under diagnosed because of the reluctance of many women to discuss their symptoms. Instead, women often self-medicate with personal hygiene products that may contain additional chemical irritants.
Dermatologists classify contact dermatitis into two categories: irritant (ICD) and allergic (ACD). ICD occurs after exposure to chemicals that directly damage skin cells. Severe ICD can cause a reaction that appears similar to a chemical burn. In contrast, allergic contact dermatitis is a true delayed hypersensitivity reaction that occurs after an initial exposure and immune sensitization to a specific allergen, followed by re-exposure. Both types of contact dermatitis can itch, although itching is more common with ACD while ICD often causes burning or stinging pain. However, even among dermatologists, it is often difficult to differentiate between ICD and ACD. Plus, both may occur simultaneously and have overlapping clinical and histological features. Identifying the specific chemical responsible for the reaction may be problematic and patch testing by a dermatologist or allergist may be required. Once diagnosed, women should be cautioned to read labels carefully, because many of these products contain similar chemicals.
Remarkable, a large number of commonly used products contain chemicals capable of causing contact dermatitis of the vulva. With the rise in the use of adult disposable moist genital wipes, most of which contain multiple fragrances and preservatives which are potential allergens or irritants, vulvar and perianal contact dermatitis is becoming increasingly common. “Unscented” products often contain a small amount of fragrance added to mask the odor of the active ingredients. To be safe from fragrance exposure, look for “fragrance-free” products.
Clinical Pearl:
Every student of medicine knows the adage: “When you hear hoof beats, think of horses, not zebras.” While that certainly applies to most patients, every so often it’s important to remember, sometimes, it is a zebra.
For a more in depth discussion of vulvar contact dermatitis see the references below.
References
- Farage MA. Vulvar susceptibility to contact irritants and allergens: a review. Arch Gynecol Obstet. 2005;272(2):167-172.
- Foote CA, Brady SP, Brady KL, Clark NS, Mercurio MG. Vulvar dermatitis from allergy to moist flushable wipes. J Low Genit Tract Dis. 2014;18(1):E16-18.
- O'Gorman SM, Torgerson RR. Allergic contact dermatitis of the vulva. Dermatitis. 2013;24(2):64-72.
- Schlosser BJ. Contact dermatitis of the vulva. Dermatol Clin. 2010;28(4):697-706.
ACM 2017 Workshops Feature All-Star Faculty Lineup
by 2017 ACM Co-Chairs
Trina Pagano MD, FACOG & Jane van Dis MD, FACOG
We are excited about our line-up of dynamic and talented speakers planned to lead this year's ACM Workshops. We chose instructors who are at the top of their fields and known for bringing innovative and creative strategies to the real-life situations we face daily as OB/GYN's and physicians. Whether you are interested in perfecting bedside ultrasound techniques, reducing the stress in your life, or dealing with conflict and improving your negotiating skills, we have an amazing workshop for you. Please join us in New Orleans to experience and learn from some of our nation's most accomplished professionals!
And, stay tuned for our September, pre-ACM newsletter where we will highlight the faculty members scheduled to lead our General Session classes.

Dr. Emmanuelle Pare
Dr. Pare joins us from Oregon Health & Science University, where she is a Maternal Fetal Medicine specialist. Dr. Pare also coordinates the resident Ob Simulation and Skills program. She has a passion for operative vaginal delivery, especially forceps and works with others to assure safe use. Dr. Pare’s course will offer a one-hour lecture reviewing the principles of safe operative vaginal delivery for both forceps and vacuum. The lecture will be followed by a skills session allowing hands on for all participants using an instrumental delivery pelvic trainer to provide a realistic experience. [ACM Faculty Page]

Dr. Jeffrey Dungan
Dr. Dungan is an Associate Professor of Clinical Genetics and Director of Ob/Gyn Ultrasound at Northwestern University. Dr. Dungan will offer a hands-on course covering common clinical scenarios encountered by the ObGyn hospitalist across the gestational-age spectrum. Ultrasound simulation stations will be used for hands-on practice and assessment. [ACM Faculty Page]

Dr. Aviad Haramati
Dr. Aviad Haramati is Professor of Integrative Physiology of the Department of Biochemistry, Molecular and Cellular Biology and Department of Medicine at Georgetown. He is the Director of Center for Innovation and Leadership in Education (CENTILE). Dr. Haramati will offer both a plenary session and as a workshop addressing stress management and resilience building for health professionals. The goal of Dr. Haramati’s workshop is to introduce participants to the reality of stress and burnout, to gain insight from the physiology of stress, and to give participants an opportunity to experience several mind-body medicine skills to gain insight to their impact and utility. [ACM Faculty Page]

Dr. Sean Esplin
Dr. Sean Esplin is an Associate Professor of Obstetrics and Gynecology at the University of Utah. Dr. Esplin's main areas of interest are the genetic control of term and preterm labor and the role of inflammation in preterm birth and he is currently involved in several ongoing research projects sponsored by the NIH aimed at identifying markers of preterm birth and obstetric complications. He also has an interest in Fetal Heart Rate Interpretation and is currently involved in several funded studies designed to evaluate protocols for interpretation and intervention on continuous FHR monitoring. [ACM Faculty Page]

Dr. Andrea Schneider
Andrea K. Schneider is a Professor of Law at Marquette University Law School where she specializes in Negotiation, Ethics, and International Conflict Resolution. She is author and co-author of numerous books in the field of dispute resolution and currently serves as co-chair of the editorial board of the ABA Dispute Resolution Magazine and on the Board of Advisors for the Saltman Center for Conflict Resolution at UNLV School of Law. Her most recent accolade, a 2017 award from ABA Section of Dispute Resolution Award for Outstanding Scholarly Work. She speaks nationally and internationally, to non-profits, corporations, law firms, and court systems and others. Most recently she has focused on faculty in the STEM and medical fields for which she has received federal grants for software development and training. Her session with SOGH will examine conflict styles, how to identify style and strategy in others, and how to negotiate effectively on behalf of one’s self or organization. [ACM Faculty Page]
Practice Matters
Physicians, like most other professionals, have life experiences that ebb and flow. At times, we dive into our professional responsibilities full throttle; other times, our personal responsibilities demand a reduction or pause in our work life. For those who have taken a break from the OB/GYN field, the process of re-entry can be daunting. This segment highlights the experience of one such physician.
By: Helen Rhodes, MD
I am 54 years old, board certified in Obstetrics & Gynecology and mother of three, "20 something year old" daughters. I come from a long line of physicians, mostly women. My maternal grandmother was a pediatrician who graduated from medical school 60 years before I did. She practiced in the UK. Two of my female cousins are physicians practicing in the UK, and my maternal uncle practiced Family Medicine in Canada. And finally, as I write this, my youngest daughter is studying for the MCAT. Striving to achieve work life balance as a female physician and raising daughters while taking care of women, has created a constant issue of re-evaluating and re-setting of my career compass since 1990. Now an empty nester, I continue to seek work life balance.I was fortunate to be spared excessive educational debt and was not the primary breadwinner for my family early in my career. Because of this, I could seek out as well as create flexible employment opportunities while my daughters were young. In fact, from 1993 through 2004, I worked part-time. Albeit, for much less income and benefits than I felt I deserved. But, my highest priority was being home as much as possible to raise my children while, at the same time, keeping my OB/GYN skills current and maintaining my board certification. In 2004, I made the decision to stop practicing obstetrics and joined the faculty of MD Anderson Cancer Center (MDA) as a benign gynecologist in a full-time position. I stayed at MDA until 2013 when I moved away from Houston and started my professional life all over again. I started a gynecology only private practice. Starting from scratch in a new community, I soon realized the resulting income deficit would need supplementation.
I have supplemented my gynecology only practice income through locum tenens and expert witness work. Unfortunately, this work is sporadic, and securing a permanent part-time position has been difficult. Many OB Hospitalist job opportunities exist, but potential employers are not keen on hiring someone like me, who hasn't delivered a baby in over ten years. In an attempt to re-enter the work force, I have offered to be "shadowed" by an existing OB hospitalist and to work for a reduced rate, until my skills meet the designated requirements. I have not found any employer willing to take on this proposal. In addition, I have researched "OB re-training" programs throughout the country but have not found one that is reasonably priced and that doesn't require substantial time away from my existing practice.
It is frustrating that I am unable to secure an opportunity to practice obstetrics, despite an inadequate supply of obstetricians currently in practice to meet the national demand for maternity care services (1). This not only places an unfair burden on the existing workforce, it also deprives the public of vital healthcare services.
I have discovered that this pause in my professional practice has amounted to a forced retirement from obstetrics. In addition, I recognize that female obstetricians are more likely to be impacted by this practice since we are the ones more likely to take this professional break.
I am disappointed that our national governing bodies such as ACOG & ABOG choose to remain quiet on this very important issue. Our field desperately needs guidance and direction for those seeking professional re-entry; guidance to the physicians, hospitals, potential employers and insurers. Currently, each hospital, employer and insurer make up their own rules and for most, the approach is to simply not hire or insure physicians who find themselves in this position.
I hope that by speaking out on this important issue, obstetrics re-training programs that are affordable and feasible may be developed. I also hope that ACOG, ABOG and other national organizations will develop standardized re-training curricula so that more physicians like myself may re-enter the obstetrics work force, practice the field we love and provide the service so desperately needed by our communities.
Reference:
Ross, Casey; STAT News, A pain in the night and a harrowing drive: A rural crisis in health care puts mothers to be on a risky road. Dr. Rhodes is a gynecologist currently practicing in Texas and is eager to restart the practice of obstetrics. ACM Early Registration Ends July 15th, 2017! ACM Early Registration Ends July 15th, 2017!
Register by 7/15/17 and save! SOGH Full members pay $475 through July 15th to attend. The registration fee covers admission to the conference and General Session lectures on Monday, Tuesday and Wednesday mornings, as well as lunch and breakfasts for those days. After July 15th, the price is $550. Don't wait. Register today!

2017 Annual Clinical Meeting Poster Contest
SOGH is pleased to present the 2nd Annual Clinical Meeting Poster Contest! This is a great opportunity for members and conference attendees to share innovations and success stories.
Suggested Poster Contest topic ideas include:
- A case report where your role as a hospitalist made a unique impact on a particular patient’s outcome – so SOGH can congratulate you for your decisive actions (don’t be shy if you did a great job!)
- A case report of an unusual presentation – it can help all of us should we encounter a similar problem
- An innovative protocol or an initiative that expanded or improved patient care – why reinvent the wheel when we can learn from each other
- Before and after data documenting the effect of an intervention on patient care – we can study the impact of our own work
Presentation Format and Eligibility Requirements:
- All Poster Contest participants must be registered for the 2017 Annual Clinical Meeting. Registration Form available here.
- All Poster Contest participants must register their poster by August 31, 2017 (there is no fee, but SOGH will ensure there is adequate space available). Register for the Poster Contest here.
- All Poster Contest participants must be present on Monday to mount their posters in the promenade area adjacent to the exhibitors and registration area on Monday and Tuesday (September 25-26).
- The poster's organizational format is flexible and appropriate to the type of your communication.
- Posters will be judged by an SOGH Panel and the top three posters will be announced on Wednesday, September 27. The poster with the greatest impact will receive an award. Contest winner must be present to win.
Poster Contest Registration Deadline: August 31, 2017
|



 Along with my colleagues, Cate Stika and Tanner Colegrove, I had the privilege of representing SOGH at ACOG’s National Summit on Women’s Health. Discussion focused on the future of our specialty, patient advocacy and resident education. Concerns were raised about the increased amount of information residents need to learn compounded by decreased work hours, and the overall effect this has on patient care. Over the past couple of decades, the number of procedures performed by graduating residents has dramatically decreased. For example, the mean number of hysterectomies performed by residents in 1980 was 175-180; in 2015 it was 90. A similar trend can be seen with forceps. The median number of FAVD performed by graduating residents in 2003 was 19 and in 2015 it decreased to five. What does this mean overall? Well, to quote Drs. Berkowitz and Minkoff: “We risk training generalists who know more and more about less and less.”
Along with my colleagues, Cate Stika and Tanner Colegrove, I had the privilege of representing SOGH at ACOG’s National Summit on Women’s Health. Discussion focused on the future of our specialty, patient advocacy and resident education. Concerns were raised about the increased amount of information residents need to learn compounded by decreased work hours, and the overall effect this has on patient care. Over the past couple of decades, the number of procedures performed by graduating residents has dramatically decreased. For example, the mean number of hysterectomies performed by residents in 1980 was 175-180; in 2015 it was 90. A similar trend can be seen with forceps. The median number of FAVD performed by graduating residents in 2003 was 19 and in 2015 it decreased to five. What does this mean overall? Well, to quote Drs. Berkowitz and Minkoff: “We risk training generalists who know more and more about less and less.”