Page 5 of 9
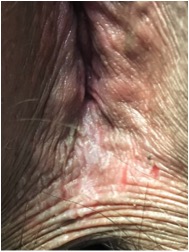
CLINICAL PEARL"When You Hear Hoof Beats, Think Horses, Not Zebras". by Cate Stika, M.D., FACOG Every student of medicine knows the adage: “When you hear hoof beats, think of horses, not zebras.” While that certainly applies to most patients, every so often it’s important to remember, sometimes, it is a zebra. A 38yo G4P2012 at 23.4 weeks of gestation presented to Ob Triage with vaginal bleeding. She reported bright red blood on the toilet tissue following both urination and defecation since intercourse 3 nights earlier. Pregnancy history was remarkable for a brief episode of vaginal spotting at 18 weeks but otherwise no other postcoital or spontaneous bleeding. She denied any change in her vaginal discharge, pelvic pressure, or contractions. A second trimester ultrasound showed a fundal placenta. A urinalysis showed 0-3 red blood cells and was otherwise negative. As I prepped for the speculum exam, the classic differential for post-coital vaginal bleeding in the mid-second trimester ran through my mind ( cervical polyp, friable cervical mucosa from a yeast or Trichomonas infection, cervical incompetence, subchorionic bleed, etc). On initial inspection, vulva appeared normal, but on closer inspection after separating the labia majora, the perinal body had diffuse lichenification with hyperkeratosis and multiple vertical fissures that had split during intercourse (see adjacent photo). The remainder of the exam was unremarkable, incl I queried the patient regarding symptoms of vulvar itching or irritation at which point she relayed that two weeks prior she had restarted using Summer’s Eve® spray, applying it to her underwear and occasionally directly onto her vulvar skin. She further reported that each time she uses this product, she develops vulvar itching after several weeks and has to temporarily stop using it. The patient was deemed stable for discharge with the diagnosis of contact dermatitis with resultant bleeding from skin breakdown. She was advised to discontinue all feminine hygiene products and recommended to use an over-the-counter topical hydrocortisone ointment once or twice daily until the fissures healed and the itching resolved. Additionally, she was recommended to apply a small amount of petroleum jelly to the area as needed several times daily to both soothe the skin and to help reduce painful exposure to urine, and rinse with cool water as needed for symptomatic relief. Discussion: Contact dermatitis was an unexpected finding in a patient who presents with 2nd trimester bleeding but fortunately a benign and easily treatable condition. For more severe reactions, a mid-to-high potency topical steroid ointment is recommended. Ointments are advised for moist vulvar skin because creams are water soluble and easily wipe off and often contain alcohols which can burn inflamed skin. It is also important to counsel women not to “overwash” because chemicals in soaps, abrasion from vigorous scrubbing and even contact with hot water can be irritating to the delicate vulvar mucosa. The vulvar skin is particularly sensitive to contact allergens and irritants. The presence of moisture, heat, pockets of occlusion, areas of friction, exposure to urine, as well as the absence of a protective keratin surface within the introitus, all contribute to the increased vulnerability of the vulvar mucosa to topical chemicals. In addition, vulvar contact dermatitis is often under diagnosed because of the reluctance of many women to discuss their symptoms. Instead, women often self-medicate with personal hygiene products that may contain additional chemical irritants. Dermatologists classify contact dermatitis into two categories: irritant (ICD) and allergic (ACD). ICD occurs after exposure to chemicals that directly damage skin cells. Severe ICD can cause a reaction that appears similar to a chemical burn. In contrast, allergic contact dermatitis is a true delayed hypersensitivity reaction that occurs after an initial exposure and immune sensitization to a specific allergen, followed by re-exposure. Both types of contact dermatitis can itch, although itching is more common with ACD while ICD often causes burning or stinging pain. However, even among dermatologists, it is often difficult to differentiate between ICD and ACD. Plus, both may occur simultaneously and have overlapping clinical and histological features. Identifying the specific chemical responsible for the reaction may be problematic and patch testing by a dermatologist or allergist may be required. Once diagnosed, women should be cautioned to read labels carefully, because many of these products contain similar chemicals. Remarkable, a large number of commonly used products contain chemicals capable of causing contact dermatitis of the vulva. With the rise in the use of adult disposable moist genital wipes, most of which contain multiple fragrances and preservatives which are potential allergens or irritants, vulvar and perianal contact dermatitis is becoming increasingly common. “Unscented” products often contain a small amount of fragrance added to mask the odor of the active ingredients. To be safe from fragrance exposure, look for “fragrance-free” products. Clinical Pearl: Every student of medicine knows the adage: “When you hear hoof beats, think of horses, not zebras.” While that certainly applies to most patients, every so often it’s important to remember, sometimes, it is a zebra. For a more in depth discussion of vulvar contact dermatitis see the references below. References
|